A chronic, partly inflammatory and partly degenerative bone condition with loss of the central load-bearing area of hyaline CARTILAGE in joints and outgrowth of cartilage at the joint margin. Eventually this cartilage reforms as new bony outgrowths known as OSTEOPHYTES. Osteophytes form with increasing age, whether or not there is significant cartilage loss, and in the elderly may lead to local frictional symptoms and, in the spine, to nerve compression.
The main clinical problems occur in the hip and knee. The cartilage loss in the hip usually occurs in the sixth or seventh decade and may affect one or both hips; such patients often have no problems in other joints. Cartilage loss in the knee occurs from the fifth decade onwards and is often associated with cartilage loss in small joints in the hand and elsewhere. Cartilage loss in the distal interphalangeal joints of the hand is associated with the formation of bony swellings known as Heberden's nodes.
Management is largely directed at maintaining activity, with physical and social support as necessary. ANALGESICS may be of some value, particularly in the management of night pain. NON-STEROIDAL ANTI-INFLAMMATORY DRUGS (NSAIDS) may help patients with early-morning stiffness and may also reduce pain on movement and night pain. Their benefit, however, tends to be less marked than in RHEUMATOID ARTHRITIS and their long-term usage has considerable toxicity problems. Advanced cartilage loss is best treated by joint replacement. Hip- and knee-joint replacements – with a wide variety of artificial joints – are operations which can greatly improve the mobility of affected individuals. (See ARTHROPLASTY.)
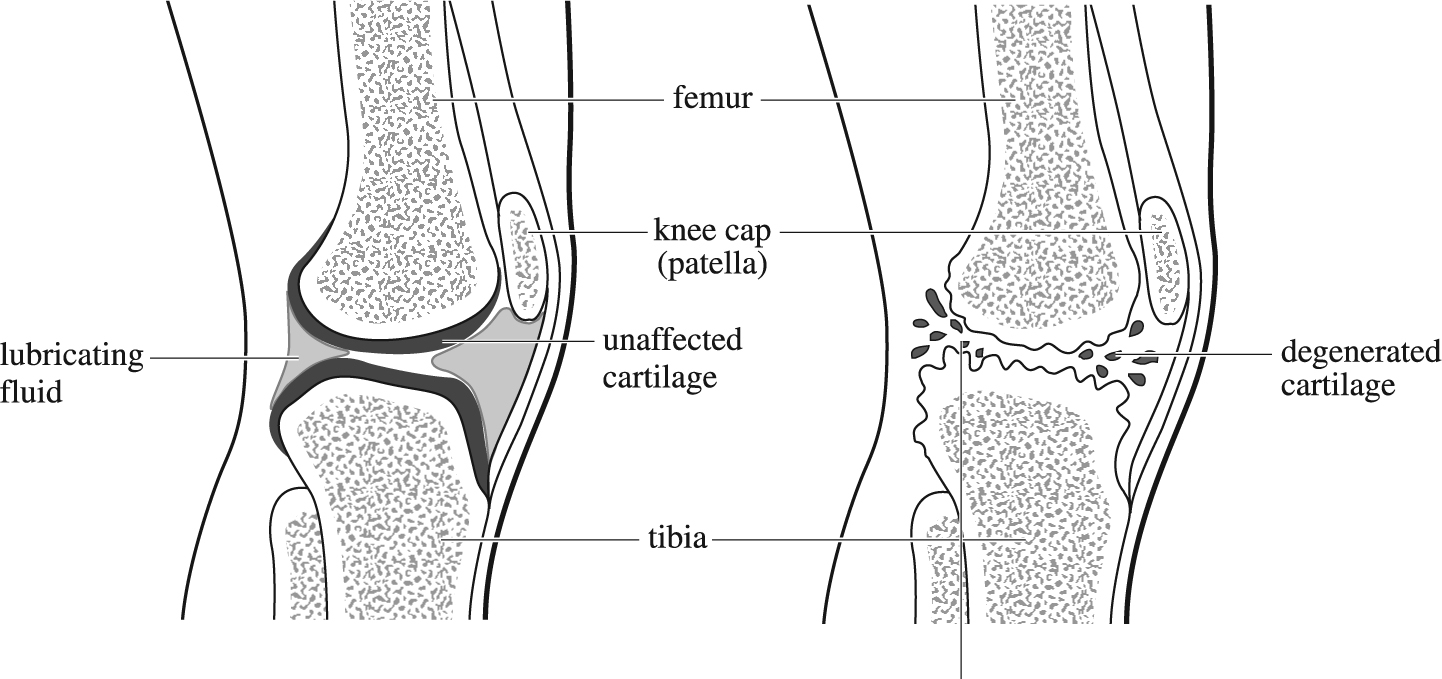
Right lateral view of vertical section through knee-joint: normal joint (left); degenerated joint cartilage and eroded bone surfaces of arthritic knee (right).