The loss or absence of sensation or feeling. Commonly used to describe a reversible process which allows operations and painful or unpleasant procedures to be performed without distress to the patient.
The speciality of anaesthesia deals with SURGERY, intensive therapy (intensive care), chronic pain management, acute pain management and obstetric analgesia. Anaesthetists in Britain are trained specialists with a medical degree, but in many countries some anaesthetists may be nurse practitioners working under the supervision of a medical anaesthetist.
The anaesthetist will assess the patient's fitness for anaesthesia, choose and perform the appropriate type of anaesthetic while monitoring and caring for the patient's well-being, and, after the anaesthetic, supervise recovery with the provision of post-operative pain relief.
Anaesthesia may be broadly divided into general and local anaesthesia. Quite commonly the two are combined to allow continued relief of pain at the operation site after the patient awakens.
is most often produced by using a combination of drugs to induce a state of reversible UNCONSCIOUSNESS. ‘Balanced’ anaesthesia uses a combination of drugs to provide unconsciousness, analgesia, and a greater or lesser degree of muscle relaxation.
A general anaesthetic comprises induction, maintenance and recovery. Historically, anaesthesia has been divided into four stages (seebelow), but these are only clearly seen during induction and maintenance of anaesthesia using inhalational agents alone.
Onset of induction to unconsciousness
Stage of excitement
Surgical anaesthesia
Overdosage
Induction involves the initial production of unconsciousness. Most often this is by INTRAVENOUS injection of a short-acting anaesthetic agent such as PROPOFOL, THIOPENTONE or ETOMIDATE, often accompanied by additional drugs such as ANALGESICS to smooth the process. Alternatively an inhalational technique may be used.
Maintenance of anaesthesia may be provided by continuous or intermittent use of intravenous drugs, but is commonly provided by administration of OXYGEN and NITROUS OXIDE or air containing a volatile anaesthetic agent. Anaesthetic machines are capable of providing a constant concentration of these, and have fail-safe mechanisms and monitors which guard against the patient's receiving a gas mixture with inadequate oxygen (see HYPOXIC). The gases are administered to the patient via a breathing circuit, either through a mask, a laryngeal mask or via ENDOTRACHEAL INTUBATION. In recent years, concerns about side-effects and pollution caused by volatile agents have led to increased popularity of total intravenous anaesthesia (TIVA).
For some types of surgery the patient is paralysed using muscle relaxants and then artificially ventilated by machine (see VENTILATOR). Patients are closely monitored during anaesthesia by the anaesthetist using a variety of devices. Minimal monitoring includes ELECTROCARDIOGRAM (ECG), blood pressure, PULSE OXIMETRY, inspired oxygen and end-tidal carbon-dioxide concentration – the amount of carbon dioxide breathed out when the lungs are at the ‘empty’ stage of the breathing cycle. Analgesic drugs (pain relievers) and local or regional anaesthetic blocks are often given to supplement general anaesthesia.
Volatile anaesthetics are halogenated ethers (isoflurane, enflurane, desflurane and sevoflurane). The latter two are the most recently introduced agents, and produce the most rapid induction and recovery – though based in many parts of the world, especially the developing world, halothane, ether and chloroform are still widely used.
Despite several theories, the mode of action of these agents is not fully understood. Their efficacy is related to how well they dissolve into the LIPID substances in nerve cells, and it is thought that they act at more than one site within brain cells – probably at the cell membrane. By whatever method, they reversibly depress the conduction of impulses within the CENTRAL NERVOUS SYSTEM and thereby produce unconsciousness.
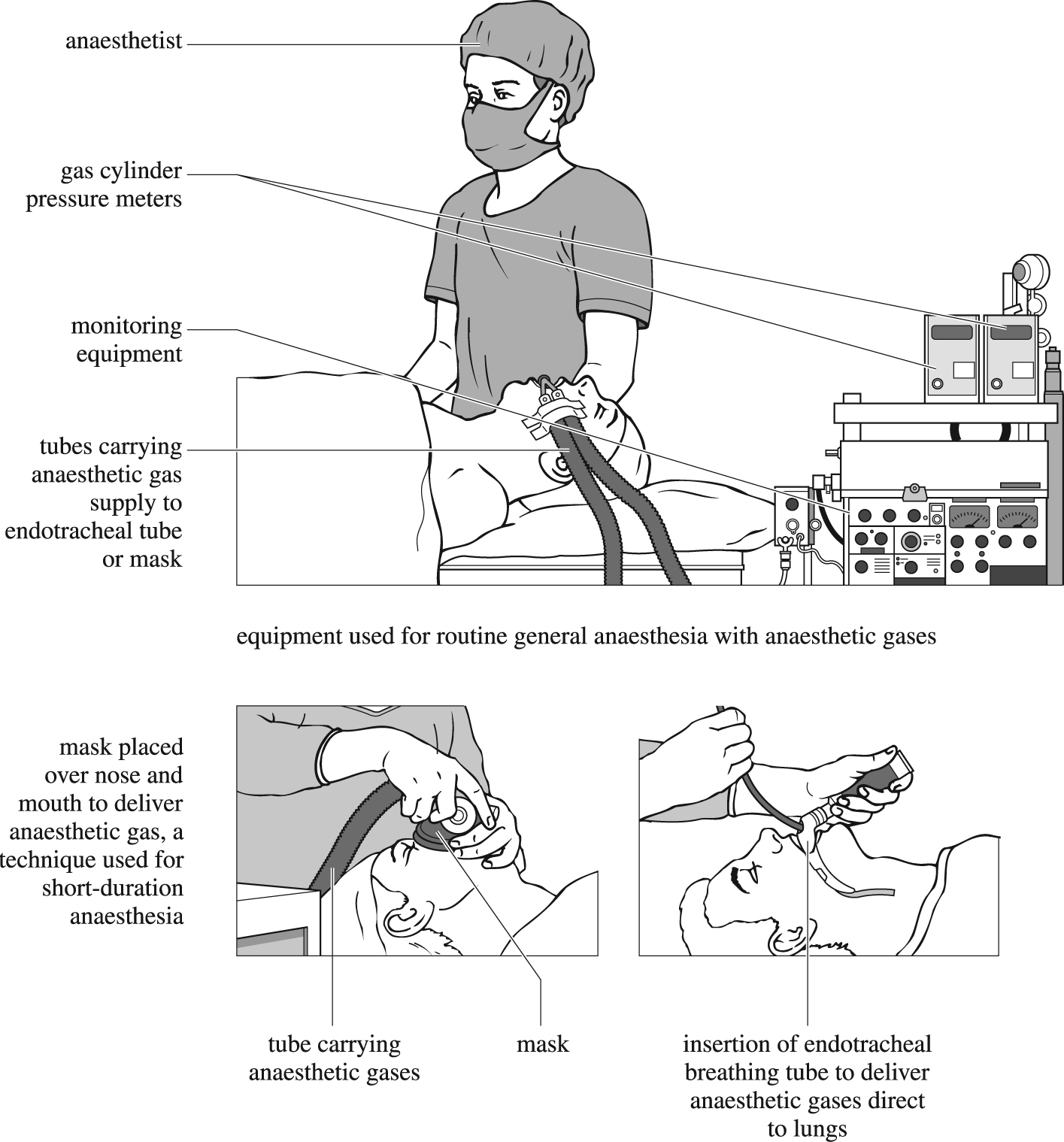
Patient under general anaesthesia (top). Use of a mask to deliver anaesthetic gases (bottom left). Delivering anaesthetic gases direct to the lungs (bottom right).
At the end of surgery any muscle relaxant still in the patient's body is reversed, the volatile agent is turned off and the patient breathes oxygen or oxygen-enriched air. This is the reversal or recovery phase of anaesthesia. Once the anaesthetist is satisfied with the degree of recovery, patients are transferred to a recovery area within the operating-theatre complex where they are cared for by specialist staff, under the supervision of an anaesthetist, until they are ready to return to the ward. (See also ARTIFICIAL VENTILATION OF THE LUNGS.)
are drugs which reversibly block the conduction of impulses in nerves. They therefore produce anaesthesia (and muscle relaxation) only in those areas of the body served by the nerve(s) affected by these drugs. Many drugs have some local anaesthetic action, but the drugs used specifically for this purpose are all amide or ester derivatives of aromatic acids. Variations in their basic structure produce drugs with different speeds of onset, duration of action and preferential SENSORY rather than MOTOR blockade (stopping the activity in the sensory or motor nerves respectively).
The use of local rather than general anaesthesia will depend on the type of surgery and in some cases the unsuitability of the patient for general anaesthesia. It is also used to supplement general anaesthesia, relieve pain in labour (see under PREGNANCY AND LABOUR) and in the treatment of pain in persons not undergoing surgery. Several commonly used techniques are listed below:
An area of anaesthetised skin or tissue is produced by injecting local anaesthetic around it. This technique is used for removing small superficial lesions or anaesthetising surgical incisions.
Local anaesthetic is injected close to a nerve or nerve plexus, often using a peripheral nerve stimulator to identify the correct point. The anaesthetic diffuses into the nerve, blocking it and producing anaesthesia in the area supplied.
Small volumes of local anaesthetic are injected into the cerebrospinal fluid through a small-bore needle which has been inserted through the tissues of the back and the dura mater (the outer membrane surrounding the spinal cord). A dense motor and sensory blockade is produced in the lower half of the body. How high up in the body it reaches is dependent on the volume and dose of anaesthetic, the patient's position and individual variation. If the block is too high, then respiratory-muscle paralysis and therefore respiratory arrest may occur. HYPOTENSION (low blood pressure) may occur because of peripheral vasodilation caused by sympathetic-nerve blockade. Occasionally spinal anaesthesia is complicated by a headache, perhaps caused by continuing leakage of cerebrospinal fluid from the dural puncture point.
Spinal nerves are blocked in the epidural space with local anaesthetic injected through a fine plastic tube (catheter) which is introduced into the space using a special needle (Tuohy needle). It can be used as a continuous technique either by intermittent injections, an infusion or by patient-controlled pump. This makes it ideal for surgery in the lower part of the body, the relief of pain in labour and for post-operative analgesia. Complications include hypotension, spinal headache (less than 1:100), poor efficacy, nerve damage (1:12,000) and spinal-cord compression from CLOT or ABSCESS (extremely rare).