or the process of eruption of the teeth in infants, may be accompanied by irritability, salivation and loss of sleep. The child will tend to rub or touch the painful area. Relief may be obtained in the child by allowing it to chew on a hard object such as a toy or rusk. A serious pitfall is to assume that an infant's symptoms of ill-health are due to teething, as the cause may be more serious. Fever and fits (see SEIZURE) are not due to teething.
is the pain felt when there is inflammation of the pulp or periodontal membrane of a tooth (see TEETH – Structure). The commonest cause is caries (see below) when the cavity is close to the pulp. Once the pulp has become infected, this is likely to spread from the apex of the tooth into the bone to form an abscess (gumboil – see below). A lesser but more long-lasting pain is felt when the dentine is unprotected. This can occur when the enamel is lost due to decay or trauma or because the gums have receded. This pain is often associated with temperature-change or sweet foods. Expert dental advice should be sought early, before the decay is extensive. If a large cavity is accessible, temporary relief may be obtained by inserting a small piece of cotton wool soaked, for example, in oil of cloves.
This is an ABSCESS caused by an infected tooth. It may be present as a large swelling or cause trismus (inability to open the mouth). Treatment is drainage of the PUS, extraction of the tooth and/or ANTIBIOTICS.
or dental decay is very common in more affluent countries and is most common in children and young adults. In the US it is said to be the most common chronic disease in children with 18 per cent of those aged 2–4, 52 per cent of those aged 6–8, and 67 per cent of 12–17 year olds being affected. In the UK, the latest figures are from a 2013 survey which showed the rates for 5 and 8 year olds in ‘milk’ teeth to be 31 per cent and 46 per cent respectively while in permanent teeth, decay had been experienced by 34 per cent of 12 year olds and 46 per cent of 15 year olds. This represents a major improvement over 20 years. At the same time, the prevalence of caries is rising alarmingly in the developing world, most likely due to dietary changes.
The cause of caries is probably acid produced by bacteria in the mouth from dietary carbohydrates, particularly refined sugar; this dissolves part of the enamel and the dentine is eroded more quickly as it is softer (see TEETH – Structure). The exposed smooth surfaces are usually protected as they are easily cleaned during normal eating and by brushing. Irregular and overcrowded teeth are more at risk from decay as they are difficult to clean.
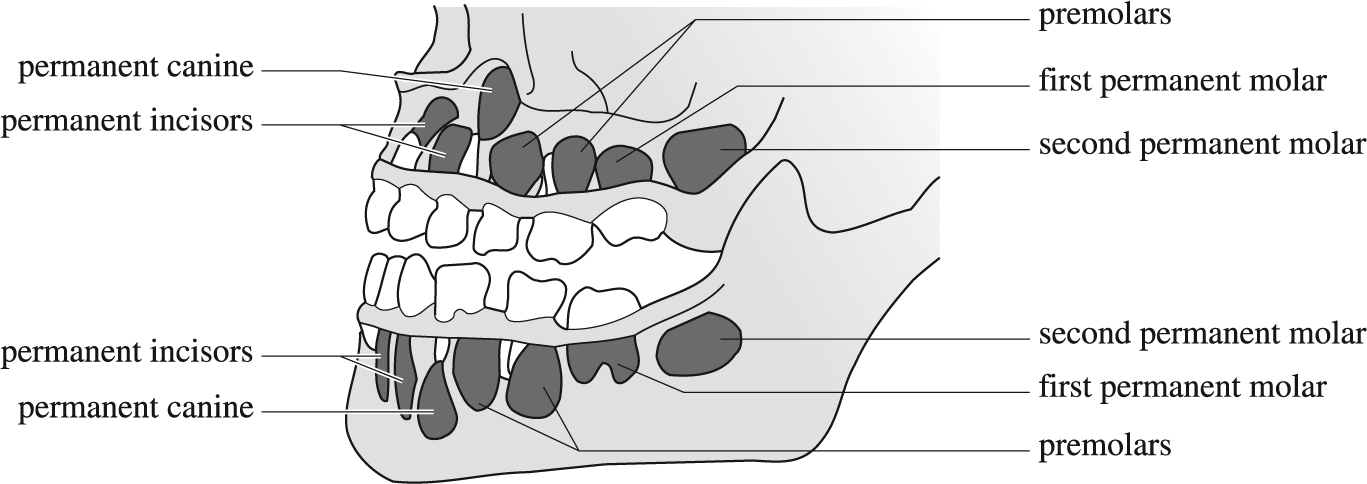
Teeth of a six-year-old child. The permanent teeth are coloured black.
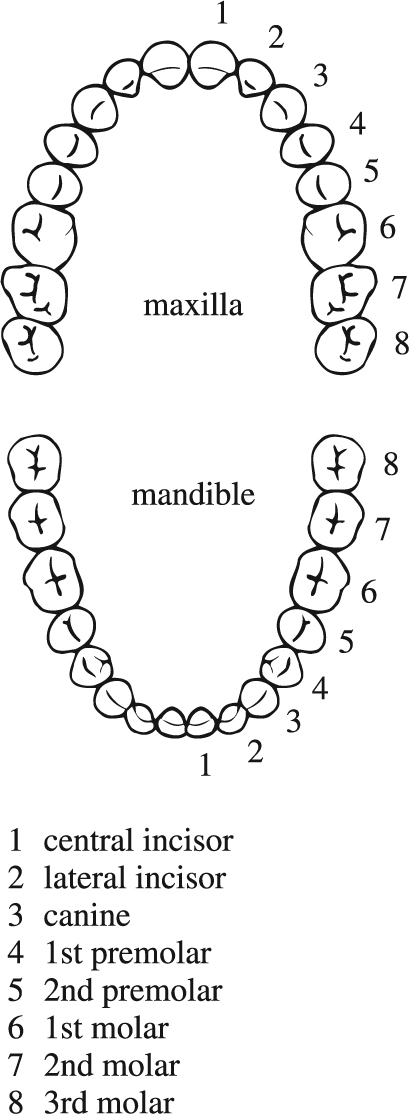
The permanent teeth of the upper (top) and lower (bottom) jaws.
Prolonged severe disease in infancy is associated with poor calcification of the teeth, making them more vulnerable to decay. As the teeth are formed and partly calcified by the time of birth, the diet and health of the mother are also important for the teeth of the child. Pregnant mothers and children should have a good balanced diet with sufficient calcium and vitamin D. A fibrous diet will also aid cleansing of the teeth and stimulate the circulation in the teeth and jaws. Fluoride in drinking water at about one part per million is associated with a reduction in the caries rate, but this is available only to about 11 per cent of children in the UK so a good adjunct/alternative is regular brushing with a fluoride toothpaste two or three times per day and certainly before going to sleep. Putting sweet or sugary juices in an infant's bottle should be avoided, and children should never be left with a bottle at night.
may be due to an abnormality in the growth of the jaws or to the early or late loss of the deciduous set (see TEETH – Development). Most frequently it is due to an imbalance in the size of the teeth and the length of the jaws. Some improvement may take place with age, but many young people need the help of an orthodontist (specialist dentist) who can correct many malocclusions by removing a few teeth to allow the others to be moved into a good position by means of springs and elastics on various appliances worn in the mouth.
may be due to an accident or inflammation of the GUM. Teeth loosened by trauma may be replaced and splinted in the socket, even if knocked right out. If loosening is due to periodontal disease, the prognosis is less favourable.
of the teeth may be intrinsic or extrinsic: in other words, the stain may be in the calcified structure or stuck on to it. Intrinsic staining may be due to JAUNDICE or the antibiotic tetracycline. Extrinsic stain may be due to tea, coffee, tobacco, pan (a mixture of chuna and betel nuts wrapped in a leaf), iron-containing medicines or excess fluoride.
or inflammation of the gum may occur as an ACUTE or CHRONIC DISORDER. The former is often part of a general infection of the mouth, and principally occurs in children or young adults, resolving after 10–14 days. The chronic form occurs later in life and tends to be progressive. Antiseptic mouthwashes may help, and once the painful stage is past, the gums should be thoroughly cleaned and any calculus removed. In severe conditions an antibiotic may be required.
is the spread of gingivitis (see above) to involve the periodontal membrane of the tooth; in its florid form it used to be called pyorrhoea. In this, the membrane becomes damaged by the inflammatory process and a space or pocket is formed into which a probe can be easily passed. As the pocket becomes more extensive, the tooth loosens. The loss of the periodontal membrane also leads to the loss of supporting bone and consequent tooth loss, difficulty in chewing and poor nutrition. Chronic inflammation soon occurs and is difficult to eradicate. Pain is not a feature of the disease but there is often an unpleasant odour (HALITOSIS). The gums bleed easily and there may be DYSPEPSIA. There may be an association with cardiovascular disease. Treatment is largely aimed at stabilising the condition rather than curing it.
is an infection that arises in or around a tooth and spreads to involve the bone. It may occur many years after a blow has killed the pulp of the tooth, or more quickly after caries has reached the pulp. At first the pain may be mild and intermittent but eventually it will become severe and a swelling will develop in the gum over the apex. A radiograph of the tooth will show a round clear area at the apex of the tooth. Treatment may be by painting the gum with a mild counter-irritant such as a tincture of aconite and iodine in the early stages, but later root-canal therapy or apicectomy may be required. If a swelling is present, it may need to be drained or the offending teeth extracted and antibiotics given.
Minor injuries include crazing and the loss of small chips of enamel, while major ones include a broken root and avulsion of the entire tooth. A specialist dental opinion should be sought as soon as possible. A tooth that has been knocked out can be re-implanted if it is clean and replaced within a few hours. It will then require splinting in place for 4–6 weeks.
As with other disorders, prevention is better than cure. Children should be taught at an early age to keep their teeth and gums clean and to avoid refined sugars between meals. It is better to finish a meal with a drink of water rather than a sweetened drink. Fluoride in some of its forms is useful whether from natural water content, artificial fluoridation where this is low and using fluoridated toothpaste. Overcrowding of the teeth, obvious maldevelopment of the jaw and persistent thumbsucking into the teens are all indications for seeking the advice of an orthodontist. Generally, adults have less trouble with decay but more with periodontal disease and, as its onset is insidious, regular dental inspections are desirable.