A benign enlargement of the THYROID GLAND with normal production of hormone. It is ENDEMIC in certain geographical areas where there is IODINE deficiency. Thus, if iodine intake is deficient, the production of thyroid hormone is threatened and the anterior PITUITARY GLAND secretes increased amounts of thyroid stimulating hormone with consequent overgrowth of the thyroid gland. Simple goitres in non-endemic areas may occur at puberty, during pregnancy and at the menopause, which are times of increased demand for thyroid hormone. The only effective treatment is thyroid replacement therapy to suppress the enhanced production of thyrotrophic hormone. The prevalence of endemic goitre can be, and has been, reduced by the iodinisation of domestic salt.
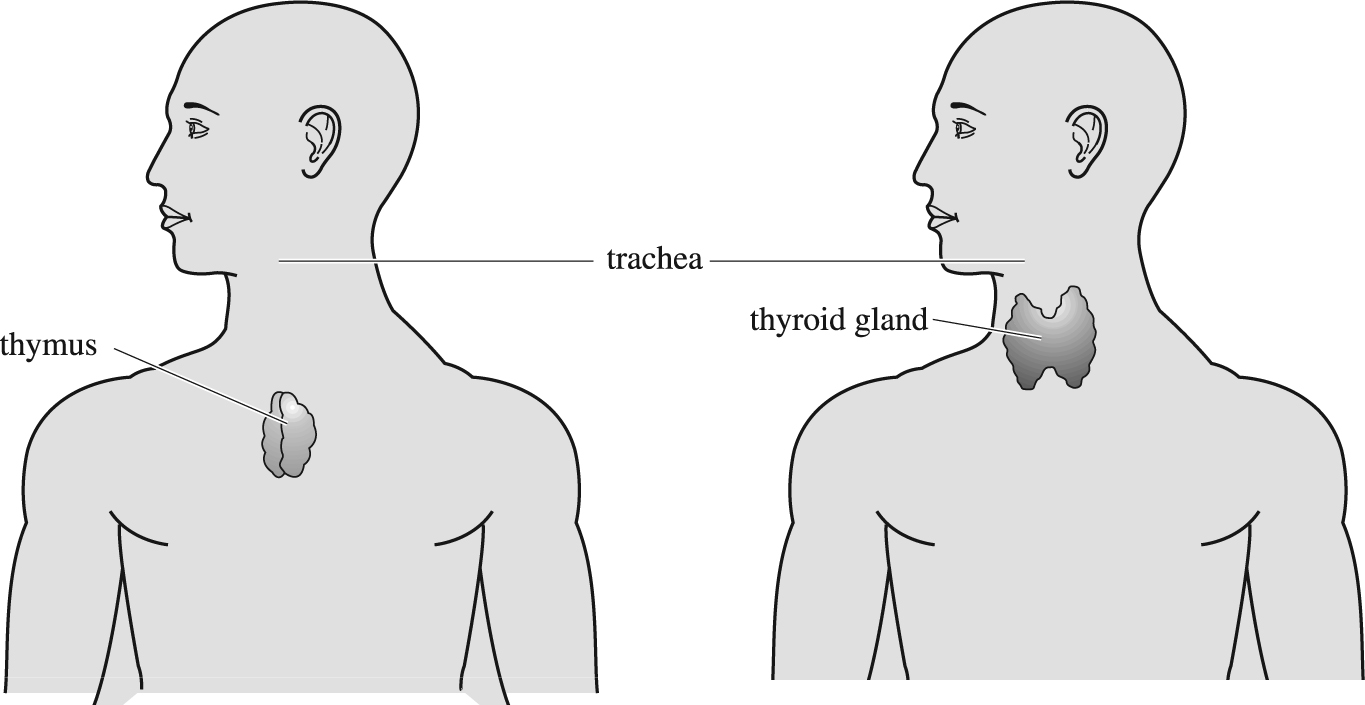
Anterior diagrammatic view showing positions of thymus (left) and thyroid (right) glands around the trachea between the lungs.
do not respond as well as the diffuse goitres to THYROXINE treatment. They are usually the result of alternating episodes of rapid growth followed by partial shrinkage which lead to permanent thyroid enlargement. The only effective way of curing a nodular goitre is to excise it, and THYROIDECTOMY should be recommended if the goitre is causing pressure symptoms or if there is a suspicion of malignancy.
are due to the production of ANTIBODIES against antigens (see ANTIGEN) in the thyroid gland. They are an example of an autoimmune disease. They tend to occur in the third and fourth decade and the gland is much firmer than the softer gland of a simple goitre. Lymphadenoid goitres respond to treatment with thyroxine.
may occur in thyrotoxicosis (see below), although much less frequently autonomous nodules of a nodular goitre may be responsible for the increased production of thyroxine and thus cause thyrotoxicosis. Thyrotoxicosis is also an autoimmune disease in which an antibody is produced that stimulates the thyroid to produce excessive amounts of hormone, making the patient thyrotoxic.
Rarely, an enlarged gland may be the result of cancer in the thyroid.
A symptomless goitre may gradually disappear or be so small as not to merit treatment. If the goitre is large or is causing the patient difficulty in swallowing or breathing, it may need surgical removal by partial or total thyroidectomy. If the patient is deficient in iodine, fish and iodised salt should be included in the diet.
is a common disorder affecting 2–5 per cent of all females at some time in their lives, but far fewer men. The most common cause – around 75 per cent of cases – is thyrotoxicosis (see below). An ADENOMA (or multiple adenomas) or nodules in the thyroid may also cause hyperthyroidism. There are also rare causes, including inflammation caused by a virus, autoimmune reactions and cancer. The symptoms of hyperthyroidism affect many of the body's systems as a consequence of the much-increased metabolic rate.
Thyrotoxicosis is a syndrome consisting of diffuse goitre (enlarged thyroid gland), overactivity of the gland and EXOPHTHALMOS (protruding eyes). Patients lose weight and develop an increased appetite, heat intolerance and sweating. They are anxious, irritable, hyperactive, suffer from TACHYCARDIA, breathlessness and muscle weakness and are sometimes depressed. The hyperthyroidism is due to the production of ANTIBODIES to the TSH receptor (see THYROTROPHIN-STIMULATING HORMONE (TSH)) which stimulate the receptor with resultant production of excess thyroid hormones. The goitre is due to antibodies that stimulate the growth of the thyroid gland. The exophthalmos is due to another immunoglobulin called the ophthalmopathic immunoglobulin, which is an antibody to a retro-orbital antigen on the surface of the retro-orbital EYE muscles. This provokes inflammation in the retro-orbital tissues which is associated with the accumulation of water and mucopolysaccharide which fills the orbit and causes the eye to protrude forwards.
Although thyrotoxicosis may affect any age-group, the peak incidence is in the third decade, presenting with a goitre, with the eye signs or, most commonly, with the symptoms of excess thyroid hormone production. Thyroid hormone controls the metabolic rate of the body so that the symptoms of hyperthyroidism are those of excess metabolism.
The diagnosis is confirmed by the measurement of the circulating levels of the two thyroid hormones, thyroxine (T4) and TRI-IODOTHYRONINE (T3).
There are several effective treatments for thyrotoxicosis.
:these drugs inhibit the iodination of tyrosine and hence the formation of the thyroid hormones. The most commonly used drugs are carbimazole and propylthiouricil: these are designed to control the excess production of thyroid hormones. Once the patient's thyroid is functioning normally, the dose is reduced to a maintenance level but may need to be continued for some years and effects may not be permanent.
:removal of three-quarters of the thyroid gland is effective treatment of thyrotoxicosis. It is the treatment of choice in those patients with large goitres. The patient must however be treated with medication so that they are euthyroid (have a normally functioning thyroid) before surgery is undertaken, or thyroid crisis and cardiac arrhythmias may complicate the operation.
:this has been in use for many years, and is an effective means of controlling hyperthyroidism. One of the disadvantages of radioactive iodine is that the incidence of hypothyroidism is much greater than with other forms of treatment, although the management of hypothyroidism is straightforward and requires only thyroxine tablets and regular blood testing. It has been the pattern in Britain to reserve radio-iodine treatment for those over the age of 35, or those whose life expectancy is unlikely to be more than 30 years as a result of cardiac or respiratory disease. Radioactive iodine treatment is not given to a seriously thyrotoxic patient.
usually PROPRANOLOL HYDROCHLORIDE: useful for symptomatic treatment during the first 4–8 weeks until the longer-term drugs have reduced thyroid activity.
A condition resulting from underactivity of the thyroid gland. One form, in which the skin and subcutaneous tissues thicken and result in a coarse appearance, is called myxoedema. The thyroid gland secretes two hormones – thyroxine and triodothyronine – and these hormones are responsible for the metabolic activity of the body. Hypothyroidism may result from developmental abnormalities of the gland, or from a deficiency of an ENZYME necessary for the synthesis of the hormones. It may be a feature of endemic goitre and retarded development, but the most common cause of hypothyroidism is the autoimmune destruction of the thyroid known as chronic thyroiditis. It may also occur as a result of radio-iodine treatment of thyroid overactivity (see above) and is occasionally secondary to pituitary disease, in which inadequate thyroid stimulating hormone (TSH) production occurs in the pituitary gland. Hyperthyroidism occurs in 14 per 1,000 females and one per 1,000 males. Most patients present between the ages of 30 and 60 years.
As thyroid hormones are responsible for the metabolic rate of the body, hypothyroidism usually presents with a general sluggishness: this affects both physical and mental activities. The intellectual functions become slow, the speech deliberate and the formation of ideas and the answers to questions take longer than in healthy people. Physical energy is reduced and patients frequently complain of lethargy and generalised muscle aches and pains. Patients become intolerant of the cold and the skin becomes dry and swollen. The LARYNX also becomes swollen and gives rise to a hoarseness of the voice. Most patients gain weight and develop constipation. The skin becomes dry and yellow due to the presence of increased carotene. Hair becomes thinned and brittle and even baldness may develop. Swelling of the soft tissues may give rise to a CARPAL TUNNEL SYNDROME and middle-ear deafness. The diagnosis is confirmed by measuring the levels of thyroid hormones in the blood, which are low, and of the pituitary TSH which is raised in primary hypothyroidism.
consists of the administration of thyroxine tablets. Treatment starts with a low dose then slowly increased to about 0.2 mg daily – the equivalent of the maximum output of the thyroid gland.
Babies may be born hypothyroid as a result of having little or no functioning thyroid-gland tissue. In the developed world the condition is diagnosed by screening, all newborn babies having a blood test to analyse TSH levels. Those found positive have a repeat test and, if the diagnosis is confirmed, start on thyroid replacement therapy within a few weeks of birth. As a result most of the ill-effects can be avoided and the children lead normal lives.
Inflammation of the thyroid gland. The acute form is usually caused by a bacterial infection elsewhere in the body: treatment with antibiotics is needed. Occasionally a virus may be the infectious agent. HASHIMOTO'S DISEASE is an autoimmune disorder causing hypothyroidism (reduced activity of the gland). Subacute thyroiditis is inflammation of unknown cause in which the gland becomes painful and the patient suffers fever, weight loss and malaise. It sometimes lasts for several months before recovery.
A variety of thyrotoxicosis (see hyperthyroidism above) in which one of the nodules of a multinodular goitre becomes autonomous and secretes excess thyroid hormone. The symptoms that result are similar to those of thyrotoxicosis, but there are minor differences.
The first line of treatment is to render the patient EUTHYROID by treatment with antithyroid drugs. Then the nodule should be removed surgically or destroyed using radioactive iodine.
A disorder of the thyroid gland in which excessive amounts of thyroid hormones are secreted into the bloodstream. Resultant symptoms are tachycardia, tremor, anxiety, sweating, increased appetite, weight loss and dislike of heat. (See hyperthyroidism above.)