Rarely, the UTERUS may be congenitally absent. In such patients secondary sexual development is normal but MENSTRUATION is absent (primary amenorrhoea). The chromosomal make-up of the patient must be checked (see CHROMOSOMES; GENES): in a few cases the genotype is male (testicular feminisation syndrome). No treatment is available, although the woman should be counselled.
The uterus develops as two halves which fuse together. If the fusion is incomplete, a uterine SEPTUM results. Such patients with a double uterus (uterus didelphys) may have fertility problems which can be corrected by surgical removal of the uterine septum. Very rarely there may be two uteri with a double vagina.
The uterus of most women points forwards (Anteversion) and bends forwards (Anteflexion). However, about 25 per cent of women have a uterus which is pointed backwards (retroversion) and bent backwards (retro flexion). This is a normal variant and very rarely gives rise to any problems. If it does, the attitude of the uterus can be corrected by VENTROSUSPENSION.
The lining of the uterine cavity is called the ENDOMETRIUM. It is this layer that is partially shed cyclically in women of reproductive age giving rise to menstruation. Infection of the endometrium is called endometritis and usually occurs after a pregnancy or in association with the use of an intrauterine contraceptive device (IUCD – see CONTRACEPTION). The symptoms are usually of pain, bleeding and a fever. Treatment is with antibiotics. Unless the FALLOPIAN TUBES are involved and damaged, subsequent fertility is unaffected.
are common. Heavy periods (menorrhagia) are often caused by fibroids (see below) or adenomyosis (see below), or by anovulatory cycles (those without release of an ovum). Anovulatory cycles result in the endometrium being subjected to unopposed oestrogen stimulation and occasionally undergoing hyperplasia. Treatment is with cyclical progestogens (see PROGESTOGEN) initially. If this form of treatment fails, endoscopic surgery to remove the endometrium may be successful. The endometrium may be removed using LASER (endometrial laser ablation) or electrocautery (TRANSCERVICAL RESECTION OF ENDOMETRIUM (TCRE)). Hysterectomy (see below) will cure the problem if endoscopic surgery fails. Adenomyosis is a condition in which endometrial tissue is found in the muscle layer (myometrium) of the uterus. It usually presents as heavy and painful periods, and occasionally pain during intercourse.
Oligomenorrhoea (scanty or infrequent periods) may be caused by a variety of conditions including thyroid disease (see THYROID GLAND, DISEASES OF). It is most commonly associated with usage of the combined oral contraceptive pill. Once serious causes have been eliminated, the patient should be reassured. No treatment is necessary unless conception is desired, in which case the patient may require induction of ovulation.
Primary amenorrhoea means that the patient has never had a period. She should be investigated, although usually it is only due to an inexplicable delay in the onset of periods (delayed menarche) and not to any serious condition. Secondary amenorrhoea is the cessation of periods after menstruation has started. The most common cause is pregnancy. It may be also caused by endocrinological or hormonal problems, tuberculous invasion of the uterine lining, emotional problems and severe weight loss. The treatment of amenorrhoea depends on the cause.
Dysmenorrhoea, or painful periods, is the most common disorder; in most cases the cause is unknown, although it may be due to excessive production of PROSTAGLANDINS.
(variations from the woman's normal menstrual pattern or changes in the duration of bleeding or the amount) can be the result of a disturbance in the balance of OESTROGENS and PROGESTERONE hormones which between them regulate the cycle. For some time after the MENARCHE or before the MENOPAUSE, menstruation may be irregular. If irregularity occurs in a woman whose periods are normally regular, it may be due to unsuspected pregnancy, early miscarriage or to disorders in the uterus, OVARIES or pelvic cavity.
Leiomyomata or fibromyoma, the commonest form of benign tumour of the uterus. They are composed of a mixture of muscular and fibrous tissue and may be small or as large as a grapefruit. Fibroids may cause pain and heavy menstrual bleeding. Small, symptomless fibroids do not need treatment but, if symptoms are unpleasant, women may choose to take anti-inflammatory and/or hormonal drugs. In others, surgery is advised.
tend to present after the age of 40 (with a peak at 55–75) with abnormal bleeding (intermenstrual or postmenopausal bleeding). They are usually endometrial carcinomas. Eighty per cent present with early (Stage I) disease. Patients with operable cancers are treated with total abdominal hysterectomy and bilateral excision of the ovaries and Fallopian tubes. Post-operative RADIOTHERAPY is usually given to those patients with adverse prognostic factors. PROGESTOGEN treatment may be extremely effective in cases of recurrence, but its value remains unproven when used as adjuvant treatment. The ten-year survival rate after treatment is about 80 per cent. In 2015 there were nearly 8,000 new cases diagnosed in the UK.
The cervix (neck of the womb) may produce an excessive discharge due to the presence of a cervical ectopy or ectropion. In both instances columnar epithelium – the layer of secreting cells – which usually lines the cervical canal is exposed on its surface. Asymptomatic patients do not require treatment. If treatment is required, cryocautery – local freezing of tissue – is usually effective.
Cervical smears are taken and examined in the laboratory to detect abnormal cells shed from the cervix. Its main purpose is to detect cervical intraepithelial neoplasia (CIN) – the presence of malignant cells in the surface tissue lining the cervix – since up to 40 per cent of women with this condition will develop cervical cancer if the CIN is left untreated. Women with abnormal smears undergo COLPOSCOPY; if CIN is found, treatment consists of simply removing the area of abnormal skin, either using a diathermy loop or laser instrument.
Cervical cancer remains the most common gynaecological cancer, with about 3,000 new cases diagnosed in the UK in 2015, with 900 deaths. Most or all would have been preventable with a successful HUMAN PAPILLOMAVIRUS IMMUNISATION programme, so the incidence of the disease can be expected to fall greatly in those countries who have such a programme. Cervical cancer is staged clinically in four bands according to how far it has extended, and treatment is determined by this staging. Stage I involves only the mucosal lining of the cervix and cone BIOPSY may be the best treatment in young women wanting children. In Stage IV the disease has spread beyond the cervix, uterus and pelvis to the URINARY BLADDER or RECTUM. For most women with stage IV, radiotherapy or radical Wertheim's hysterectomy – the latter being preferable for younger women – is the treatment of choice if the cancer is diagnosed early, both resulting in survival rates of five years in 80 per cent of patients. Patients with cervical cancer are usually offered concurrent CHEMOTHERAPY and radiotherapy if they present too late for surgery or if the surgical skill to perform a radical hysterectomy is not available. These operations are best performed by gynaecological oncologists who are surgeons specialising in the treatment of gynaecological tumours.
is a disorder in which the organ drops from its normal situation down into the vagina. First-degree prolapse is a slight displacement of the uterus, second-degree a partial displacement and third-degree when the uterus can be seen outside the VULVA. It may be accompanied by a CYSTOCOELE (the bladder bulges into the front wall of the vagina), urethrocoele (the urethra bulges into the vagina) and rectocoele (the rectal wall bulges into the rear wall of the vagina). Prolapse most commonly occurs in middle-aged women who have had children, but the condition is much less common now than in the past when prenatal and obstetric care was poor, women had more pregnancies and their general health was poor. Treatment is with pelvic exercises, surgical repair of the vagina or hysterectomy. If the woman does not want or is not fit for surgery, an internal support called a pessary can be fitted – and changed periodically.
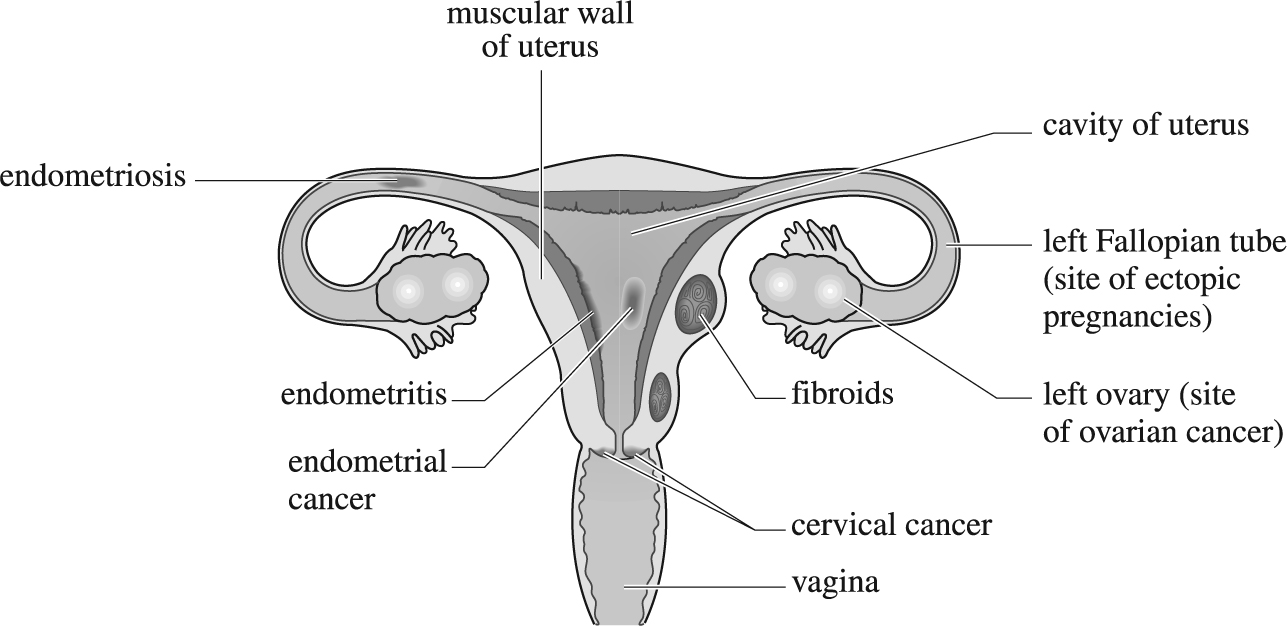
Vertical section of female reproductive tract (viewed from front) showing sites of common gynaecological disorders.
Many serious conditions of the uterus have traditionally been treated by hysterectomy, or removal of the uterus. It remains a common surgical operation in the UK, but is being superseded in the treatment of some conditions, such as persistent MENORRHAGIA, with drug treatment (levonorgestrel releasing intrauterine system, TRANEXAMIC ACID or combined ORAL CONTRACEPTIVEs), endometrial ablation – removal of the lining of the uterus using minimally invasive techniques, usually using an ENDOSCOPE and laser. NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE (NICE) regards hysterectomy as a last resort for women with heavy menstrual bleeding. The operation may be necessary, however to treat cancer of the uterus and cervix, ENDOMETRIOSIS and sometimes for severely prolapsed uterus. Total hysterectomy is the usual type of operation: it involves the removal of the uterus and cervix and sometimes the ovaries. After hysterectomy a woman no longer menstruates and cannot become pregnant. If the ovaries have been removed as well and the woman had not reached the menopause, HORMONE REPLACEMENT THERAPY (HRT) should be considered.